Health Secretary promises improved cancer care in deprived areas
Wes Streeting vows to end the postcode lottery of cancer care with more training and technology
More doctors will be able to train to become cancer specialists at NHS trusts in deprived areas of England under Government plans to end a postcode lottery in cancer care.
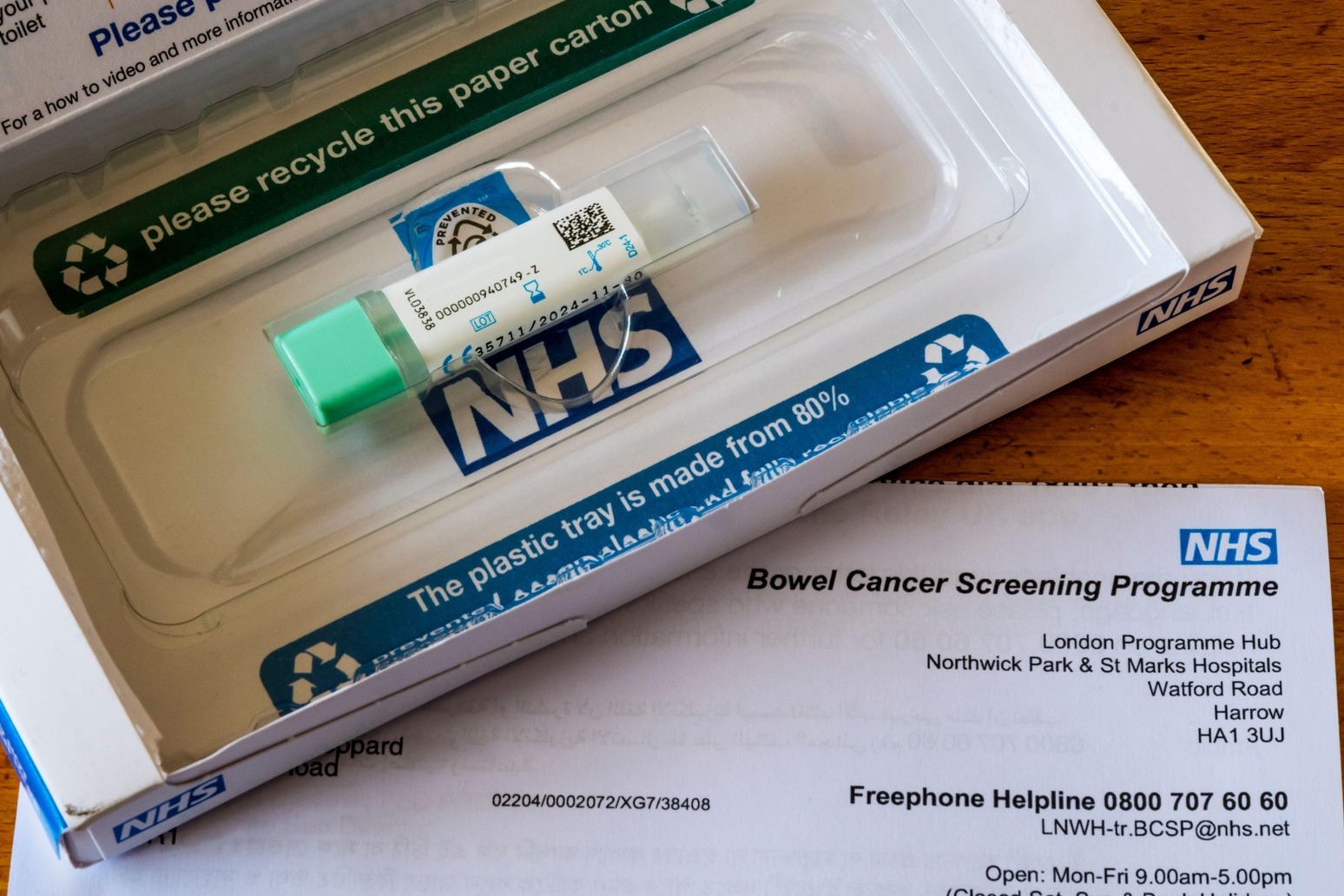
A raft of new tests and technologies to spot cases of the disease earlier will also be assessed by the NHS spending watchdog to determine if they can be rolled out in the health service.
The measures form part of the Government’s upcoming National Cancer Plan, a strategy that will aim to prevent cancer, speed up diagnosis and enhance treatment.
Under the plans, the Government will introduce new training places for medics at under-served NHS trusts, with a focus on rural and coastal areas.
Health Secretary Wes Streeting said patients in these communities deserve “the same shot at survival and quality of life as everyone else”.
Ministers will also work with the royal colleges to entice more doctors to specialise in clinical and medical oncology in a bid to boost numbers.
Meanwhile, from April 2027, new tests and devices that help spot cancer sooner will be assessed by the National Institute for Health and Care Excellence (Nice).
The move will help roll out these technologies in the NHS faster, according to the Department of Health and Social Care.
Mr Streeting said: “For too long, your chances of seeing a doctor and catching cancer early have depended on where you live. That’s not fair and has to stop.
“I am determined to end the health inequalities that have grown across England over the last 15 years. We’re training more doctors in the communities that need them most and making sure the latest cancer detection technology reaches every corner of the country.
“Faster diagnosis doesn’t just save lives – it gets people back to work and back to their families sooner.
“Whether you live in a coastal town or a rural village, you deserve the same shot at survival and quality of life as everyone else. This government will turn that promise into a reality.”
The first tests and devices to be assessed by Nice under the new model include artificial intelligence that reads chest X-rays to help medics spot lung cancer, software that analyses tissue samples for prostate and breast cancer to speed up diagnosis, and new techniques to help women get answers about unexplained vaginal bleeding.
Nice will also assess the “sponge on a string” test for oesophageal cancer.
It involves patients swallowing a small capsule attached to a string, which dissolves in the stomach to leave a small sponge about the size of a 1p coin.
This is then pulled out after a few minutes, collecting cells from the oesophageal lining for analysis.
Professor Jonathan Benger, chief executive of Nice, said: “When Nice was founded 26 years ago, it set out to end the postcode lottery in access to medicines. We’re now extending that same clarity and fairness to health tech.
“These reforms mean that clinically and cost-effective medical devices, diagnostics and digital tools will start to be reimbursed and made available consistently across the NHS.
“This will give patients faster access to proven technologies and ensure NHS resources are spent where they make the greatest difference.”
Last week, NHS England’s monthly performance figures showed that 76.5% of patients urgently referred for suspected cancer were diagnosed or had cancer ruled out within 28 days in November, up from 76.1% in October and above the current target of 75%.
However, there continues to be a large difference between the proportion of patients having the disease ruled out and those having it confirmed.
Some 78.0% of those patients ruled out of having cancer were told within 28 days in November but just 55.1% of patients had their cancer confirmed within 28 days.
The proportion of patients who had waited no longer than 62 days in November from an urgent suspected cancer referral, or consultant upgrade, to their first definitive treatment for cancer was 70.2%, up from 68.8% in October.
The Government and NHS England have set a target of March 2026 for this figure to reach 75%.
Steven McIntosh, chief partnerships officer at Macmillan Cancer Support, said: “Right now, cancer care isn’t fair.
“Too many aren’t getting the treatment and care they need because of who they are and where they live, and rural and coastal communities often have the worst outcomes.
“The National Cancer Plan for England is a huge opportunity to break down the barriers to everyone accessing world class cancer care.”
Prof Peter Johnson, national clinical director for cancer at NHS England, said the National Cancer Plan will tackle differences in care “head-on”.
According to Cancer Research UK, there are more than 168,000 cancer deaths in the UK every year – the equivalent of about 460 a day.
Michelle Mitchell, chief executive of Cancer Research UK, said: “No-one should be at a greater risk of dying of cancer because of where they live, but cancer death rates are around a third higher for people living in the most deprived areas of England compared to the least deprived.
“It’s right for the UK Government to tackle this – action is needed to boost the number of cancer specialists in the places that need them most, so everyone can be treated as quickly as possible.
“Ensuring everybody across England can access the best diagnostic tests is also crucial.
“Beating cancer must mean beating it for everybody, and the National Cancer Plan for England has a huge opportunity to bring us closer to this goal.
Published: by Radio NewsHub